Our Services  General Surgery
General Surgery  Weight Management and Metabolic Surgery Service
Weight Management and Metabolic Surgery Service
The Weight Management and Metabolic Surgery Service of Hong Kong Sanatorium & Hospital provides long-term solutions for patients who struggle with their weight and metabolic disorders.
The comprehensive service is supported by multidisciplinary expertise from surgeons, endocrinologists, dietitians, physiotherapists, clinical psychologists, plastic surgeons, anaesthetists and nursing specialists. Together we offer advanced surgical, endoscopic, pharmacological and lifestyle modification options to achieve the goals of sustained weight loss, cure of metabolic disorders and better quality of life.
Obesity
Obesity is a disease. It is a disorder of energy regulation of our body, which is manifested as change of body contour resulting from excessive accumulation of fat. It is not a simple cosmetic problem as perceived in the past. According to 2018 data from the Department of Health of Hong Kong SAR, 50% of the population has a body mass index (BMI) > 23kg/m2 (defined as overweight) or > 25kg/m2 (defined as obese).
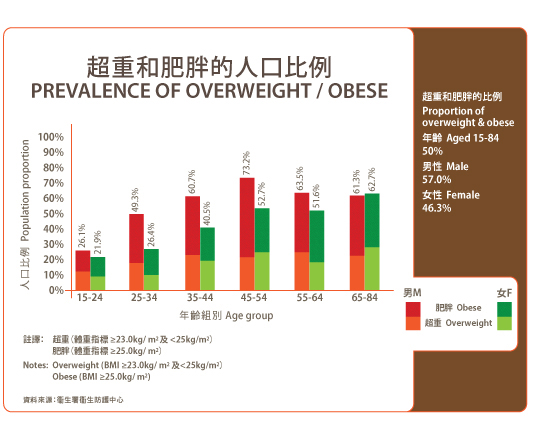
Figure 1. Prevalence of Overweight/Obese (2018 Data from Centre for Health Protection, Department of Health)
How to measure obesity:
Body mass index (BMI) = body weight in kg / body height in meter square (kg/m2).
| Generalised obesity | Asian | Western population |
| Normal | BMI 18-22.9 kg/m2 | BMI 18.5-24.9kg/m2 |
| Overweight | BMI 23-24.9 kg/m2 | BMI 25-29.9 kg/m2 |
| Obesity | BMI =/> 25 kg/m2 | BMI =/> 30 kg/2 |
| Abdominal obesity | ||
| Men | WC* > 90 cm | WC > 102 cm |
| Women | WC >80 cm | WC > 88cm |
Table 1. Criteria of Obesity
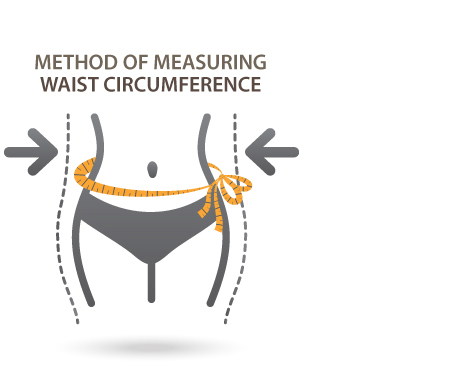
Figure 2. Method of measuring waist circumference
Body composition is also a reference of obesity. Healthy body composition is listed in figure 3 and table 2.
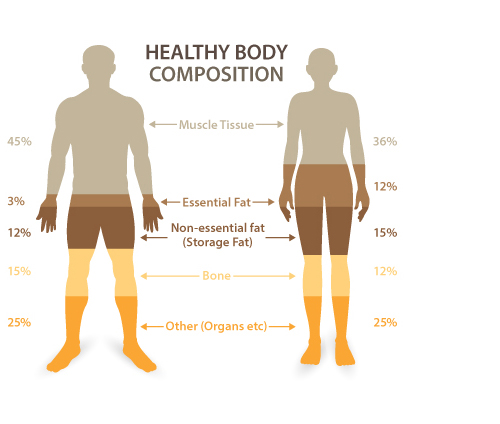
Figure 3. Healthy body composition
Excessive accumulation of fat is an index of obesity.
Body Fat Percentage
| Description | Men | Women |
| Essential fat | 2-5% | 10-13% |
| Athletes | 6-13% | 14-20% |
| Fitness | 14-17% | 21-24% |
| Average | 18-24% | 25-31% |
| Obese | >25% | >32% |
Causes of obesity
There are multiple factors that can lead to obesity. To put it simply, excessive energy may accumulate as fat deposit inside the body if one takes in more calories than one expends. Factors leading to obesity can be genetic, environmental and behavioural, and they also include endocrine or metabolic disorders.
Obesity is easily observed in members of the same family. Patients who inherit the obese gene tend to be less responsive to a leptin hormone (lean hormone) from fat cells. Eating habits within the same family may also contribute to obesity when consumption of high-energy content food is the usual eating style. Junk food consumption and sedentary lifestyle could be other reasons. Patient with some diseases are prone to suffering problems associated with obesity, such as depression, Bulimia Nervosa, Binge Eating Disorder, hypothyroidism, Cushing syndrome. Medications including steroids and anti-depressant may also cause obesity.
Obesity-associated health problems
More obese patients are associated with a higher risk of developing comorbidities.
| BMI (kg/m2) | Risk of comorbidities | ||
| Waist circumference < 90cm (M) < 80cm (F) |
Waist circumference >/= 90cm (M) >/=80cm (F) |
||
| Normal weight | 18.5-22.9 | Average | Increased |
| Overweight | 23 | ||
| At risk | 23-24.9 | Increased | Moderate |
| Obese I | 25-29.9 | Moderate | Severe |
| Obese II | >30 | Severe | Very severe |
Co-morbidities associated with obesity (energy regulation disorders) are listed in figure 4.
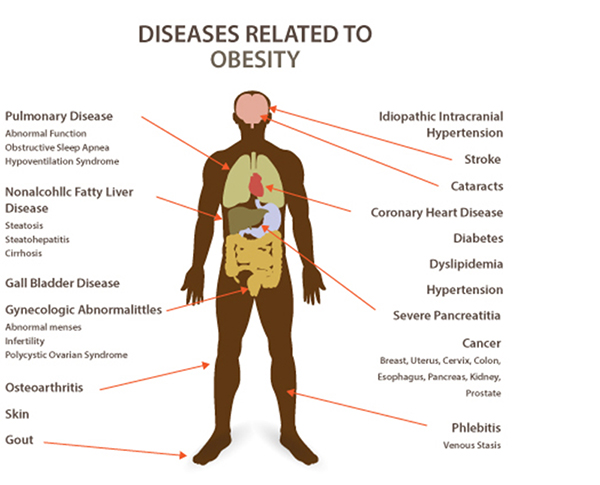
Figure 4. Diseases related to obesity.
As a result of all the possible co-morbidities associated with obesity, life expectancy of an obese patient is estimated to be 5-20 years shorter than the non-obese general population.
Metabolic syndrome
Conceptually, metabolic syndrome is a collection of medical diseases risk factors that lead to increased chance of developing ischaemic heart disease, stroke and diabetes and thus a shortened life expectancy. International Diabetes Federation (IDF) has recently launched a new definition of metabolic syndrome:
Central obesity (measured by waist circumference):
Asian (Japanese excluded) : >/=90cm (men), >/=80cm (women)
Plus at least two of the following factors:
- Triglycerides >1.7mmol/L (150mg/dL)
- High-density lipoprotein (HDL) cholesterol <1.03mmol/L (40mg/dL) in men, <1.29 (50mg/dl) in women
- Blood pressure >/=130/85 or on treatment
- Fasting blood glucose (FBG) >5.6mmol/L or previously diagnosed diabetes
Solutions to obesity, metabolic syndrome and diabetes
We strive to combat obesity, metabolic syndrome and type 2 diabetes by various methods with individualised formulated strategy by our team of expertise. The goal of weight control is not limited to improving body weight and appearance, but also improves general health status by ameliorating or curing obesity-related comorbidities.
We provide detailed evaluation for patients who wish to improve their healthy status by body weight management. An individualsed therapeutic strategy is formulated after evaluation.
Solution to obesity
The methods to control body weight include dieting, exercise and lifestyle modification, pharmacotherapy and interventional treatment, such as surgery.
Diet, exercise and lifestyle modification
This is regarded as first line of treatment as well as a crucial component for body weight maintenance after achieving target by any other treatment modalities. Lifestyle modification per se, however, is not effective for severely obese patients. It has been proven in large-scale studies that only 5-10% of patients can successfully maintain the ideal body weight after a few years.
The success rate will improve under professional expertise, such as those from a dietitian and physiotherapist, guidance and close monitoring. Dietitians and physiotherapists in Hong Kong Sanatorium & Hospital are dedicated to providing a professional and tailor-made programme for patients who are interested in using lifestyle modification therapeutic strategy.
Pharmacotherapy
Medication therapy for overweight or obesity does not replace dieting, exercise and a healthy lifestyle. In general, patients who use medication lose 3-9% weight more than those who adopt lifestyle modification alone. However, not everyone is suitable for medication control. Children, the elderly older than 70 years of age, especially those with multiple medical diseases, and pregnant women are not advised to use medication to control body weight. Potentially, the drugs might have side effects and one should expect to regain some weight once the treatment is stopped.
Drugs act by suppressing your appetite, reducing nutrient absorption or increasing excretion of energy (sugar) out of your body.
Interventional Treatment
Service scope
- Metabolic and bariatric surgeries
- Laparoscopic sleeve gastrectomy
- Single incision sleeve gastrectomy
- Laparoscopic gastric plication
- Lap-band revision
- Laparoscopic Roux-en-Y gastric bypass
- Laparoscopic sleeve gastrectomy plus duodenojejunal bypass
- Laparoscopic sleeve gastrectomy plus proximal jejunal bypass
- Revisional metabolic and bariatric surgery
- Endoscopic metabolic and bariatric surgery
- Intra-gastric balloon placement
- Aspiration therapy
- Endoscopic sleeve gastroplasty
- Endoscopic revision of bariatric procedures
- Medical weight control service
- Medication with weight monitoring program
- Life-style modification service
- Diet education and monitoring
- Exercise education and monitoring program
- Body-contouring and personal image service
- Pre-interventional / treatment education and counselling
- Post-operative / treatment weight loss monitoring and maintenance counselling
Interventional Therapy for Obesity, Type 2 Diabetes and Metabolic Syndrome
Obesity
According to different severity of obesity, there are different options for the treatment of obesity. Diet and exercise are recommended for overweight and mildly obese patients. Pharmacotherapy is also appropriate for selected patients under specialist supervision. Interventional therapeutic options are available for a more robust effect and can be classified as reversible or irreversible.
Intragastric balloon
Intragastric balloon is a reversible option. An intragastric balloon can be placed inside the stomach and 400-700ml fluid was injected to inflate the balloon. The procedure is performed by endoscopy under intravenous sedation or monitored anaesthesia. It works by occupying part of volume of gastric cavity to produce easy fullness after diet and make one eat less food. The balloon needs to be taken out 6 months to 1 year after placement. Patient can expect to lose 12-15kg during the treatment period. However, the body weight of around 70% of patients will rebound after balloon retrieval. There is no limitation on BMI cut-off value as indication for treatment but it is usually for patients who are not fit for surgery/mildly obese or it is used as bridging therapy for those super obese before they formally undergo surgery.
Endoscopic surgery
Numerous endoscopic procedures are evolving but most of them are still under research investigation on safety and efficacy. These procedures, e.g. endoscopic gastroplasty, are performed totally by endoscopy. The stomach is sutured to a smaller size. For safety reason, most of these innovative procedures are performed under research purpose.
Bariatric surgery
The most commonly performed procedures are laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass. Laparoscopic adjustable gastric banding was once very popular but is now seldom performed in most parts of the world owing to the long-term risk profile.
Sleeve gastrectomy
It has become the most commonly performed procedure globally. The procedure is easy, safe and with minimal long-term complications. Most patients undergo this procedure and enjoy excellent postoperative quality of life. The weight loss effect is due to restrictive component of the stomach, as 60-70 percent of the greater curve side of the stomach is resected, turning the stomach into a banana shape. The amount of food intake will reduce, thus leading to weight reduction. An additional effect of sleeve gastrectomy is that the where hunger hormone-secreting fundus is resected. Patients after sleeve gastrectomy will feel significantly less hungry and has no more food-craving behavior.
Roux-en-Y gastric bypass
This procedure involves restrictive and malabsorptive components. Distal portion of stomach is separated from the proximal stomach. Proximally, a 60-100ml pouch is created and a distal segment of small bowel is connected to it. Food after ingestion will soon pass to distal small bowel and bypass the stomach and duodenum. Eating amount and length of small bowel for absorption are reduced, thereby inducing weight reduction. The procedure is slightly more complex and has a slightly higher complication rate when compared with sleeve gastrectomy.
When do I need bariatric / metabolic surgery?
Indication for bariatric / metabolic surgery mainly depends on three factors:
1. Your body mass index (BMI) BMI calculator:-----------
2. Presence of type 2 diabetes (T2DM)
3. Presence of metabolic syndrome
According to International Federation for the Surgery of Obesity and Metabolic Disorders -Asia Pacific Chapter (IFSO-APC) consensus statements 2011, bariatric / metabolic surgery should be considered if:
1. BMI >/= 35kg/m2 with or without co-morbidities.
2. BMI >/=30kg/m2 with T2DM or metabolic syndrome, when T2DM or metabolic syndrome inadequately controlled by life-style modification or medication.
3. BMI >/=27.5kg/m2, surgery as non-primary alternative to treatment T2DM or metabolic syndrome.
When the purpose of surgery is to treat diabetes, international guidelines are as follows:
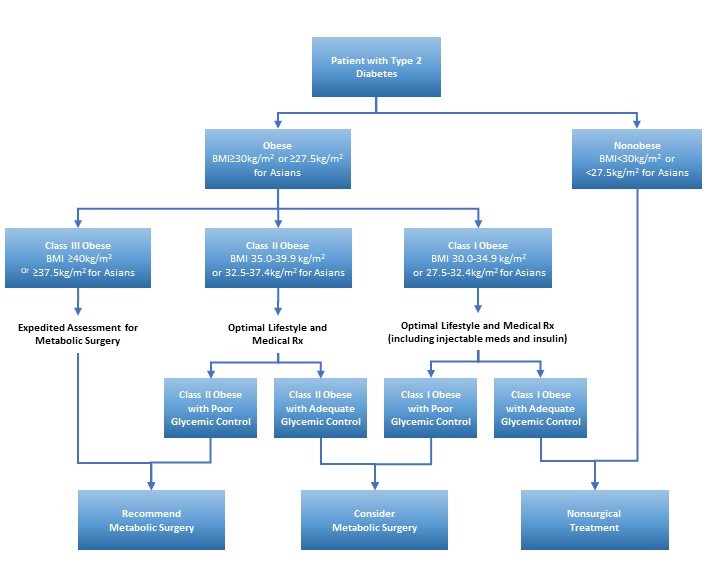
Diabetic Surgery / Metabolic Surgery
Surgery has been recognised internationally as a standard treatment modality for type 2 diabetes in appropriately selected patients. In the second Diabetes Surgery Summit in 2016, it was demonstrated with strong scientific evidence that the gastrointestinal tract constitute a crucial role in metabolic regulation. Alteration of anatomy of gastrointestinal tract achieves excellent glycaemic control and reduces microvascular and macrovascular complications of diabetes, thus reducing incidence of diabetic nephropathy, diabetes- induced stroke and cardiovascular diseases. Metabolic surgery is recommended for patients with BMI >37.5kg/m2 and those with BMI 32.5-37.5kg/m2 when hyperglycaemia is inadequately controlled by lifestyle and optimal medical therapy. Surgery should be considered for patients with BMI 27.5-32.5kg/m2 if hyperglycaemia is inadequately controlled despite optimal treatment with right oral or injectable medications.
When should surgery be done?
To put it simply, metabolic surgery should be done as soon as possible if indicated.
Due to its invasiveness, many people perceive surgery as the last resort after exhaustion of all other treatment modalities. However, diabetes is a progressively degenerative disease due to its natural course of progression. The glycaemic control after surgery relies on endocrine function of the pancreas. If the disease deteriorates to terminal stage when all islet cells / endocrine function of pancreas burn out, surgery will also be ineffective. Therefore, gastrointestinal metabolic surgery is not effective for type 1 diabetes. Hence, surgery should be performed early to stop degenerative disease progression.
Currently, scientific evidence proves age (the younger, the better), BMI (the higher, the more effective), C-peptide (preferably > 50% of function preserved) and duration of diabetes (preferrably <5 years) are important factors to predict the glycaemic effect of surgery.
Is diabetic / metabolic surgery only effective for obesity and diabetes?
Metabolic surgery is also effective for hypertension, hyperlipidemia, fatty liver, obesity caused obstructive sleep apnea to various extents. Risks of diabetic nephropathy, stroke and cardiovascular diseases are lowered. Risks of obesity-related cancers such as cardia, colon, rectum, breast and endometrium cancers are also minimised and life expectancy is expected to improve.
Choice of surgical procedure
Depending on the purpose (to treat obesity or medical disease), a patient’s general condition and efficacy of each treatment option, your doctor will discuss with you the best surgical procedure that suits you. For example, patients with pre-existing gastroesophageal reflux may not be suitable for sleeve gastrectomy whereas for those who wish for treatment of diabetes, a gastric balloon may not be the best option. Patients with uncontrolled psychiatric conditions are also not suitable for surgery.
Why is surgery effective in treating diabetes and metabolic syndrome?
The mechanism of surgery that brings about improvements on medical diseases is complex. Each procedure has a unique mechanism. Intragastric balloon, for example, reduces body weight by limiting the amount of food intake. The improvement on medical diseases is the result of losing body weight, and the effect is relatively mild.
The mechanism of laparoscopic sleeve gastrectomy is much more complex: the hunger hormone-secreting fundus of the stomach is resected, making the patients feel less hungry after sleeve gastrectomy. With the tubular shape of the neo-gastric tube, the duration of food staying in the stomach is short and it will pass to distal gut soon after ingestion. This induces expedited secretion of insulin after meal and better control of blood glucose. Insulin resistance also improves after surgery and after further weight loss.
Scientifically, it has demonstrated that alteration of gastrointestinal anatomy induces changes of gastrointestinal hormones, bile acid, gut microbiota, etc. in metabolic surgical procedures.
Is surgery is risky? Will it leave scars?
The risk of surgery is low, i.e. comparable to a simple laparoscopic cholecystectomy. Main short-term risks include staple line bleeding and leak, and they are less than 5%. Mortality risk is less than 0.1%. Long-term risks include gastroesophageal reflux, stomal ulcer, vitamin trace element deficiency and internal organ herniation, but the rate of incidence is low.
All procedures are performed with a minimally invasive approach or single incision. Scar pictures
Will life be permanently changed after surgery?
Our expert team of dietitians and physiotherapists will guide you through post-operative rehabilitation. Usually, the first three months after operation is called “lifestyle re-modeling period”. Our dietitians will teach you on eating method, e.g. eat slowly and chew slowly before swallowing. Choosing low-calorie food is also important. Exercise is also an indispensable component of rehabilitation. Our professional physiotherapists will guide you on the method of exercise and intensity. Once a healthy lifestyle habit is entrenched, you will find that body weight maintenance is not as difficult as you may imagine.
Frequently Asked Questions:
- What is the cost of treatment?
It depends on what kind of treatment you need. Structured treatment programmes with are listed with prices in the website.
- Will insurance cover my treatment cost?
Insurance reimbursement after treatment is not guaranteed. In the past, treatment for obesity is mostly excluded by insurance companies or in most insurance policies. It is because obesity has been regarded as a result of weak self-regulation, minimal self-discipline and lack of diet control and exercise. However, obesity and metabolic disorders have been regarded as energy regulation disorders. Patients are not the one totally to be blamed. There are many successful cases of insurance reimbursement. Most of these patients underwent treatment because of medical reason and were regarded as medical essential. Treatment approaches were complied with international practice guidelines. Metabolic surgery, in particular, prevents patients from future major diseases claims such as renal dialysis, stroke or myocardia infraction attack that are more expensive.
- What is the age limit for surgery?
Extremes of age:
The usual age eligible for bariatric and metabolic surgery ranges from 18-70. Patients below 18 are evaluated individually and according to paediatric parameters. The lowest age limit for surgical intervention is 16. Age below this should be assessed by a paediatrician to exclude other problems including behavioral, congenital or hormonal disorders.
Elderly above 70 are usually associated with multiple medical diseases, and the benefits of surgery are outweighed by the risks. Invasive interventional will be offered only under exceptional condition.
- My family has several obese members. Am I likely to be benefit from surgery?
There are two potential reasons for this situation: first, the family members have a similar lifestyle; second, a genetic reason. Surgery can help control the body weight and is probably the only method for a sustained body weight. Children born after weight reduction are usually not obese.
- I am planning for pregnancy. Should I get pregnant before or after the surgery?
Obese mothers will usually give birth to obese children, while those of mothers with a normal weight are healthier and usually have a normal body weight.
Bariatric surgery is not advisable during pregnancy. Patients are advised not to get pregnant within 1 year after surgery.
- I have gained a lot of weight during pregnancy. Are there any methods to help me regain my body figure?
Postpartum obesity can usually be managed by monitored lifestyle modification. Our professional dietitians and physiotherapists provide dedicated programmes to help you achieve this purpose. Various interventional options are readily available to help the minority of patients who are not able to return to healthy status.
- I have diabetes for many years. I wish to have it cured. Is it possible?
It depends on your body condition. If you are young with adequate pancreatic endocrine function but obese, there is still a significant chance to ameliorate your diabetes by interventional treatment.
Patient Journey
- Arrive at Hong Kong Sanatorium & Hospital
- Consult our dietitian at Dietetics Centre
- Basic vital signs and parameter assessment (BMI) +/- body composition analysis
- Patient education by a case manager / nurse specialist
a. Join a Diet /Exercise/Introductory Package
b. Refer to a Surgeon (for all potential surgical candidates)
c. Refer to an Endocrinologist (for candidates interested in pharmacotherapy)
- Surgery
- Postoperative follow-up